Published :
Updated :
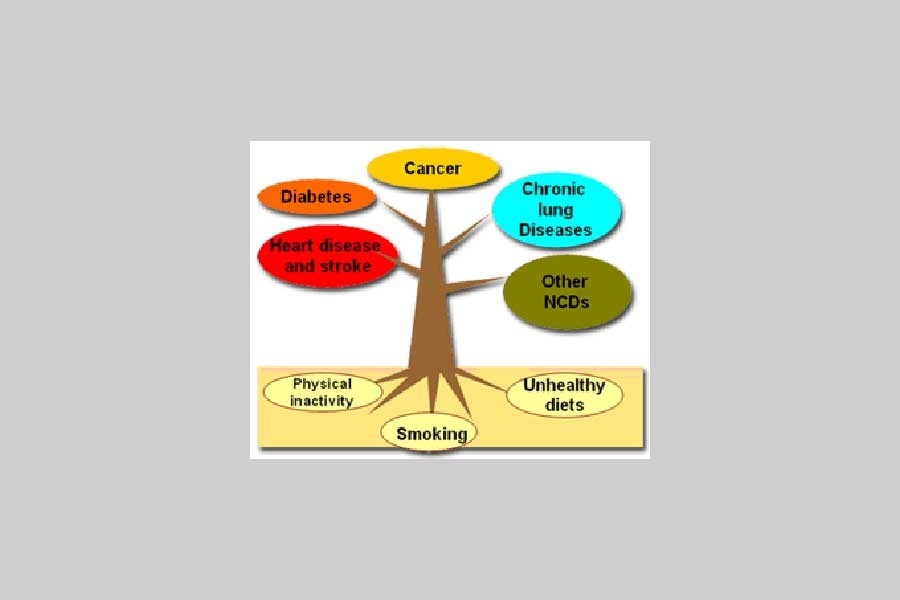
Setting up the NCD (non-communicable diseases) units in the upazila health complexes of the country some years ago was a praiseworthy move. It did promise to ease suffering of the rural people from various non-communicable diseases. In the absence of basic treatment facilities, patients in rural areas have no choice but to move to specialised hospitals and clinics in district headquarters or to those in the capitsal Dhaka which in most cases are far beyond their affordability. The NCD units were meant to provide medical help to patients locally at affordable costs. Between 2007 and 2010, these were opened at the upazila health complexes to provide treatment to increasing number of chronic patients suffering from respiratory diseases, diabetes, hypertension, cardiovascular diseases etc. In a scenario where 70 per cent of the country's population are not covered by healthcare services provided by the state, these small units at the upazila level looked like ushering in a new era in heathcare servicing for the masses.
However, a recent study on the functioning of the NCD units speaks of the crippling situation these are in due mainly to fund crunch, unavailability of basic tools and materials, and last but not least, dearth of doctors. The study found that besides dedicated and trained doctors, nurses, technologists and other support staff, these medical units suffer from shortage of equipment and testing facilities, logistics and drug supplies. More than anything, lack of coordination between the NCD units and the central NCD wing reflects endemic systemic problems.
The mega project, despite its country-wide presence in most upazilas, was not at all too ambitious given the basic infrastructure available in the upazila heath complexes-to start with. The main idea that prompted setting up of the NCD units was to give treatment for ailments common to poor people in rural areas, which account for 59 per cent of deaths annually. The government's National Health Bulletin data show that most of the deaths at hospitals are caused by cardiac complications, brain hemorrhage, chronic respiratory diseases, cancer, diabetes and other non-communicable diseases. Understandably, not all such ailments can be expected to be addressed in the NCD units. However, providing primary treatment or referring the patients to district-level or other healthcare service centres could have been a commendable job. Things did not turn the way they should have.
As it now appears, fund crunch is a major problem. While such difficulty is so common to big initiatives such as this, it is not at all clear how the government initially planned to run it. Obviously, lack of fund is also responsible for its inability to do enough to institutionalise the NCD-related services. Given that the country-wide project has great merit and usefulness to the overwhelming majority of the people, the authorities should look into the loopholes in the system and put up their best in order that the NCD units are made meaningfully functional and not put on the back burner. Seeking support of development partners could be an option that the government can explore.

 For all latest news, follow The Financial Express Google News channel.
For all latest news, follow The Financial Express Google News channel.